Acute coronary syndrome (ACS) refers to a spectrum of clinical presentations ranging from those for ST-segment elevation myocardial infarction (STEMI) to presentations found in non–ST-segment elevation myocardial infarction (NSTEMI) or in unstable angina. It is almost always associated with rupture of an atherosclerotic plaque and partial or complete thrombosis of the infarct-related artery.
Essential update: ACC/AHA Guidelines on the management of non-ST-elevation acute coronary syndromes
The American College of Cardiology/American Heart Association (ACC/AHA) released the following guidelines recommendations on the management of non-ST-elevation ACSs to assist in maximizing patient outcomes :
- Patients with chest pain or other symptoms suggesting acute coronary syndromes (ACS) should have 12-lead electrocardiography (ECG) performed and evaluated within 10 min of arrival at an emergency facility, and serial ECGs should be performed to detect ischemic changes.
- Serial cardiac troponin I or T levels (using a contemporary assay) should be obtained at presentation and at 3-6 hr after symptom onset. Risk scores can help assess prognosis.
- In patients with symptoms consistent with ACS without objective evidence of myocardial ischemia (nonischemic ECG and normal cardiac troponin levels), noninvasive imaging is reasonable before emergency department discharge or within 72 hr after discharge.
- Standard initial medical therapies include supplemental oxygen for arterial oxygen saturation < 90% or respiratory distress; sublingual nitroglycerin; oral beta-blocker therapy within the first 24 hr in the absence of heart failure, low output state, increased risk for cardiogenic shock, or other contraindications to beta-blockade; nondihydropyridine calcium channel blocker for continuing or recurrent ischemia and contraindication to beta-blockade (in the absence of clinically significant left ventricular dysfunction).
- Nonsteroidal anti-inflammatory drugs (except aspirin) should not be initiated and should be discontinued during the hospitalization for NSTE-ACS because of the increased risk of major adverse cardiac events associated with their use.
- Initial antiplatelet/anticoagulant therapy includes 325-mg chewable aspirin at presentation, followed by a daily maintenance dose of aspirin at 81-126 mg daily. A P2Y12 inhibitor (clopidogrel or ticagrelor) should be used in addition to aspirin for up to 12 mo in patients treated with either an early-invasive or ischemia-guided strategy. In addition to antiplatelet therapy, parenteral anticoagulation is indicated with enoxaparin, bivalirudin, fondaparinux, or unfractionated heparin.
- A high-intensity statin should be initiated or continued in all patients without contraindications. Angiotensin-converting enzyme inhibitors should be started and continued indefinitely with a left ventricular ejection fraction ≤40% or hypertension, diabetes, or stable chronic kidney disease unless contraindicated.
- An early invasive strategy is indicated for patients with refractory angina or hemodynamic or electrical instability and those at elevated risk for clinical events. An early invasive strategy is not recommended for patients with extensive comorbidities (eg, hepatic, renal, or pulmonary failure; cancer) in whom the risks of revascularization and comorbid conditions are likely to outweigh the benefits of revascularization. An ischemia-guided strategy is appropriate for low–risk score patients (Thrombolysis In Myocardial Infarction or Global Registry of Acute Coronary Events), for low-risk troponin-negative women, and by patient or clinician preference in the absence of high-risk features. When an ischemia-guided strategy is chosen, noninvasive stress testing is recommended prior to hospital discharge to detect severe ischemia occurring at a low-stress threshold.
- Patients undergoing percutaneous coronary intervention (PCI) should be treated with a P2Y12 inhibitor: clopidogrel, prasugrel, or ticagrelor. Discharge planning should include detailed patient education about symptoms, lifestyle interventions, standard medication with dual antiplatelet therapy, cholesterol management, referral to cardiac rehabilitation, timely follow-up with the healthcare team, and influenza and pneumococcal vaccines.
- NSTE-ACS patients with prior revascularization PCI or coronary artery bypass grafting should receive antiplatelet and anticoagulant therapy and be strongly considered for an early invasive strategy because of their increased risk. Medical treatment in the acute phase of NSTE-ACS and decisions to perform stress testing, angiography, and revascularization should be similar in patients with and without diabetes mellitus.
- Patients who develop NSTE-ACS following noncardiac surgery should receive guideline-directed medical therapy, with additional management directed at the underlying cause of the pathophysiologic process.
- Older patients with NSTE-ACS, because of their high-risk status, should be treated with guideline-directed medical therapy and an early invasive strategy with revascularization as appropriate; pharmacotherapy should be individualized and dose adjusted by weight and creatinine clearance to reduce adverse events. Management decisions should be patient centered, incorporating patient preferences, comorbidities, functional and cognitive status, and life expectancy.
- Women with NSTE-ACS should be managed with the same pharmacologic therapy as men for acute care and secondary prevention, with attention to weight and/or renally calculated doses of antiplatelet and anticoagulant agents to reduce bleeding risk. Women with NSTE-ACS and high-risk features (eg, troponin positive) should undergo an early invasive strategy.
Signs and symptoms
Atherosclerosis is the primary cause of ACS, with most cases occurring from the disruption of a previously nonsevere lesion. Complaints reported by patients with ACS include the following:
- Palpitations
- Pain, which is usually described as pressure, squeezing, or a burning sensation across the precordium and may radiate to the neck, shoulder, jaw, back, upper abdomen, or either arm
- Exertional dyspnea that resolves with pain or rest
- Diaphoresis from sympathetic discharge
- Nausea from vagal stimulation
- Decreased exercise tolerance
Physical findings can range from normal to any of the following:
- Hypotension: Indicates ventricular dysfunction due to myocardial ischemia, myocardial infarction (MI), or acute valvular dysfunction
- Hypertension: May precipitate angina or reflect elevated catecholamine levels due to anxiety or to exogenous sympathomimetic stimulation
- Diaphoresis
- Pulmonary edema and other signs of left heart failure
- Extracardiac vascular disease
- Jugular venous distention
- Cool, clammy skin and diaphoresis in patients with cardiogenic shock
- A third heart sound (S 3) and, frequently, a fourth heart sound (S 4)
- A systolic murmur related to dynamic obstruction of the left ventricular outflow tract
- Rales on pulmonary examination (suggestive of left ventricular dysfunction or mitral regurgitation)
Potential complications include the following:
- Ischemia: Pulmonary edema
- Myocardial infarction: Rupture of the papillary muscle, left ventricular free wall, and ventricular septum
Diagnosis
Guidelines for the management of non-ST-segment elevation ACS were released in 2011 by the European Society of Cardiology (ESC). The guidelines include the use of the CRUSADE risk score (Can Rapid risk stratification of Unstable angina patients Suppress ADverse outcomes with Early implementation of the ACC/AHA guidelines).
In the emergency setting, electrocardiography (ECG) is the most important diagnostic test for angina. ECG changes that may be seen during anginal episodes include the following:
- Transient ST-segment elevations
- Dynamic T-wave changes: Inversions, normalizations, or hyperacute changes
- ST depressions: These may be junctional, downsloping, or horizontal
Laboratory studies that may be helpful include the following:
- Creatine kinase isoenzyme MB (CK-MB) levels
- Cardiac troponin levels
- Myoglobin levels
- Complete blood count
- Basic metabolic panel
Diagnostic imaging modalities that may be useful include the following:
- Chest radiography
- Echocardiography
- Myocardial perfusion imaging
- Cardiac angiography
- Computed tomography, including CT coronary angiography and CT coronary artery calcium scoring
Management
Initial therapy focuses on the following:
- Stabilizing the patient’s condition
- Relieving ischemic pain
- Providing antithrombotic therapy
Pharmacologic anti-ischemic therapy includes the following:
- Nitrates (for symptomatic relief)
- Beta blockers (eg, metoprolol): These are indicated in all patients unless contraindicated
Pharmacologic antithrombotic therapy includes the following:
- Aspirin
- Clopidogrel
- Prasugrel
- Ticagrelor
- Glycoprotein IIb/IIIa receptor antagonists (abciximab, eptifibatide, tirofiban)
Pharmacologic anticoagulant therapy includes the following:
- Unfractionated heparin (UFH)
- Low-molecular-weight heparin (LMWH; dalteparin, nadroparin, enoxaparin)
- Factor Xa inhibitors (rivaroxaban, fondaparinux)
Additional therapeutic measures that may be indicated include the following:
- Thrombolysis
- Percutaneous coronary intervention (preferred treatment for ST-elevation MI)
Current guidelines for patients with moderate- or high-risk ACS include the following:
- Early invasive approach
- Concomitant antithrombotic therapy, including aspirin and clopidogrel, as well as UFH or LMWH
See Treatment and Medication for more detail.
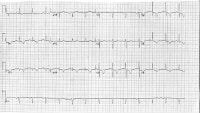
The image below depicts a 62-year-old woman with a history of chronic stable angina and a "valve problem."
 A 62-year-old woman with a history of chronic stable angina and a "valve problem" presents with new chest pain. She is symptomatic on arrival, complaining of shortness of breath and precordial chest tightness. Her initial vital signs are blood pressure = 140/90 mm Hg and heart rate = 98. Her electrocardiogram (ECG) is as shown. She is given nitroglycerin sublingually, and her pressure decreases to 80/palpation. Right ventricular ischemia should be considered in this patient.
A 62-year-old woman with a history of chronic stable angina and a "valve problem" presents with new chest pain. She is symptomatic on arrival, complaining of shortness of breath and precordial chest tightness. Her initial vital signs are blood pressure = 140/90 mm Hg and heart rate = 98. Her electrocardiogram (ECG) is as shown. She is given nitroglycerin sublingually, and her pressure decreases to 80/palpation. Right ventricular ischemia should be considered in this patient.Background
Acute coronary syndrome (ACS) refers to a spectrum of clinical presentations ranging from those for ST-segment elevation myocardial infarction (STEMI) to presentations found in non–ST-segment elevation myocardial infarction (NSTEMI) or in unstable angina. In terms of pathology, ACS is almost always associated with rupture of an atherosclerotic plaque and partial or complete thrombosis of the infarct-related artery. (See Etiology.)
In some instances, however, stable coronary artery disease (CAD) may result in ACS in the absence of plaque rupture and thrombosis, when physiologic stress (eg, trauma, blood loss, anemia, infection, tachyarrhythmia) increases demands on the heart. The diagnosis of acute myocardial infarction in this setting requires a finding of the typical rise and fall of biochemical markers of myocardial necrosis in addition to at least 1 of the following (See Workup.):
- Ischemic symptoms
- Development of pathologic Q waves
- Ischemic ST-segment changes on electrocardiogram (ECG) or in the setting of a coronary intervention
The terms transmural and nontransmural (subendocardial) myocardial infarction are no longer used because ECG findings in patients with this condition are not closely correlated with pathologic changes in the myocardium. Therefore, a transmural infarct may occur in the absence of Q waves on ECGs, and many Q-wave myocardial infarctions may be subendocardial, as noted on pathologic examination. Because elevation of the ST segment during ACS is correlated with coronary occlusion and because it affects the choice of therapy (urgent reperfusion therapy), ACS-related myocardial infarction should be designated STEMI or NSTEMI. (See Workup.)
Attention to the underlying mechanisms of ischemia is important when managing ACS. A simple predictor of demand is rate-pressure product, which can be lowered by beta blockers (eg, metoprolol or atenolol) and pain/stress relievers (eg, morphine), while supply may be improved by oxygen, adequate hematocrit, blood thinners (eg, heparin, IIb/IIIa agents such as abciximab, eptifibatide, tirofiban, or thrombolytics), and/or vasodilators (eg, nitrates, amlodipine). (See Medications.)
In 2010, the American Heart Association (AHA) published new guideline recommendations for the diagnosis and treatment of ACS.
Etiology
Acute coronary syndrome (ACS) is caused primarily by atherosclerosis. Most cases of ACS occur from disruption of a previously nonsevere lesion (an atherosclerotic lesion that was previously hemodynamically insignificant yet vulnerable to rupture). The vulnerable plaque is typified by a large lipid pool, numerous inflammatory cells, and a thin, fibrous cap.
Elevated demand can produce ACS in the presence of a high-grade fixed coronary obstruction, due to increased myocardial oxygen and nutrition requirements, such as those resulting from exertion, emotional stress, or physiologic stress (eg, from dehydration, blood loss, hypotension, infection, thyrotoxicosis, or surgery).
ACS without elevation in demand requires a new impairment in supply, typically due to thrombosis and/or plaque hemorrhage.
The major trigger for coronary thrombosis is considered to be plaque rupture caused by the dissolution of the fibrous cap, the dissolution itself being the result of the release of metalloproteinases (collagenases) from activated inflammatory cells. This event is followed by platelet activation and aggregation, activation of the coagulation pathway, and vasoconstriction. This process culminates in coronary intraluminal thrombosis and variable degrees of vascular occlusion. Distal embolization may occur. The severity and duration of coronary arterial obstruction, the volume of myocardium affected, the level of demand on the heart, and the ability of the rest of the heart to compensate are major determinants of a patient's clinical presentation and outcome. (Anemia and hypoxemia can precipitate myocardial ischemia in the absence of severe reduction in coronary artery blood flow.)
A syndrome consisting of chest pain, ischemic ST-segment and T-wave changes, elevated levels of biomarkers of myocyte injury, and transient left ventricular apical ballooning (takotsubo syndrome) has been shown to occur in the absence of clinical CAD, after emotional or physical stress. The etiology of this syndrome is not well understood but is thought to relate to a surge of catechol stress hormones and/or high sensitivity to those hormones.
Baseline blood glucose levels appear to be an independent risk factor for a major adverse cardiac event (MACE) in emergency department (ED) patients with suspected ACS. In an analysis of data from 1708 Australian and New Zealand patients in a prospective observational study, investigators noted a MACE occurred within 30 days of presentation in 15.3% of patients whose ED admission blood glucose levels were below 7 mmol/L (about 126 mg/dL); however, in the same time period, a MACE occurred in twice as many patients (30.9%) whose blood glucose levels were above 7 mmol/L. After controlling for various factors, patients who had admission blood glucose levels of 7 mmol/L or higher were at 51% higher risk of experiencing a MACE compared with patients who had lower baseline blood glucose levels. Other significant predictors of MACE included male sex, older age, family history, hypertension, dyslipidemia, ischemic findings on ECG, and positive troponintests.
Prognosis
Six-month mortality rates in the Global Registry of Acute Coronary Events (GRACE) were 13% for patients with NSTEMI ACS and 8% for those with unstable angina.
An elevated level of troponin (a type of regulatory protein found in skeletal and cardiac muscle) permits risk stratification of patients with ACS and identifies patients at high risk for adverse cardiac events (ie, myocardial infarction, death) up to 6 months after the index event (See Workup.)
The PROVE IT-TIMI trial found that after ACS, a J-shaped or U-shaped curve association is observed between BP and the risk of future cardiovascular events.
LeLeiko et al determined that serum choline and free F(2)-isoprostane are also predictors of cardiac events in ACS. The authors evaluated the prognostic value of vascular inflammation and oxidative stress biomarkers in patients with ACS to determine their role in predicting 30-day clinical outcomes. Serum F(2)-isoprostane had an optimal cutoff level of 124.5 pg/mL, and serum choline had a cutoff level of 30.5 µmol/L. Choline and F(2)-isoprostane had a positive predictive value of 44% and 57% and a negative predictive value of 89% and 90%, respectively.
Testosterone deficiency is common in patients with coronary disease and has a significant negative impact on mortality. Further study is needed to assess the effect of treatment on survival.
A study by Sanchis et al suggests renal dysfunction, dementia, peripheral artery disease, previous heart failure, and previous myocardial infarction are the comorbid conditions that predict mortality in NSTEMI ACS. In patients with comorbid conditions, the highest risk period was in the first weeks after NSTEMI ACS. In-hospital management of patients with comorbid conditions merits further investigation.
Patients with end-stage renal disease often develop ACS, and little is known about the natural history of ACS in patients receiving dialysis. Gurm et al examined the presentation, management, and outcomes of patients with ACS who received dialysis before presentation for an ACS. These patients were enrolled in the Global Registry of Acute Coronary Events (GRACE) at 123 hospitals in 14 countries from 1999-2007.
NSTEMI ACS was the most common in patients receiving dialysis, occurring in 50% of patients (290 of 579) versus 33% (17,955 of 54,610) of those not receiving dialysis The in-hospital mortality rates were higher among patients receiving dialysis (12% vs 4.8%; p < 0.0001). Higher 6-month mortality rates (13% vs 4.2%; p < 0.0001), recurrent myocardial infarction incidence (7.6% vs 2.9%; p < 0.0001), and unplanned rehospitalizations (31% vs 18%; p < 0.0001) were found among those who survived to discharge. Outcomes in patients who received dialysis was worse than was predicted by the calculated GRACE risk score for in-hospital mortality (7.8% predicted vs 12% observed; p < 0.05). This suggests that the GRACE risk score underestimated the risk of major events in these patients.
In a study that assessed the impact of prehospital time on STEMI outcome, Chughatai et al suggest that “total time to treatment” should be used as a core measure instead of “door-to-balloon time.” This is because on-scene time was the biggest fraction of "pre-hospital time.” The study compared groups with total time to treatment of more than 120 minutes compared with 120 minutes or less and found mortalities were 4 compared with 0 and transfers to a tertiary care facility were 3 compared with 1, respectively.
STEMI mechanisms and stenting outcome similar in women and men
Despite their smaller coronary vessels and higher risk profile, women with STEMI appear to respond just as well as men to primary PCI and stenting, according to the Optical Coherence Tomography Assessment of Gender Diversity in Primary Angioplasty (OCTAVIA) study. OCTAVIA, which was designed to examine gender differences at the time of primary PCI, included 140 STEMI patients at 14 Italian centers, matched by age and risk factors, who received an everolimus-eluting stent.
On initial OCT, no differences by gender were found in the proportion of ruptured or eroded plaques, thus suggesting that the pathophysiology of STEMI is nearly identical in men and women. On repeat OCT at nine months, intended to assess stent healing, more than 90% of both men and women had fully covered stent struts. Although OCTAVIA was not powered for clinical end points, no significant differences in death, reinfarction, stroke, stent thrombosis, or target vessel reintervention were evident at one year.
Patient Education
Patient education of risk factors is important, but more attention is needed regarding delays in door-to-balloon time, and one major barrier to improving this delay is patient education regarding his or her symptoms. Lack of recognition of symptoms may cause tremendous delays in seeking medical attention.
Educate patients about the dangers of cigarette smoking, a major risk factor for coronary artery disease (CAD). The risk of recurrent coronary events decreases 50% at 1 year after smoking cessation. Provide all patients who smoke with guidance, education, and support to avoid smoking. Smoking-cessation classes should be offered to help patients avoid smoking after a myocardial infarction. Bupropion increases the likelihood of successful smoking cessation.
Diet plays an important role in the development of CAD. Therefore, prior to hospital discharge, a patient who has had a myocardial infarction should be evaluated by a dietitian. Patients should be informed about the benefits of a low-cholesterol, low-salt diet. In addition, educate patients about AHA dietary guidelines regarding a low-fat, low-cholesterol diet.
A cardiac rehabilitation program after discharge may reinforce education and enhance compliance.
The following mnemonic may useful in educating patients with CAD regarding treatments and lifestyle changes necessitated by their condition:
- A = Aspirin and antianginals
- B = Beta blockers and blood pressure (BP)
- C = Cholesterol and cigarettes
- D = Diet and diabetes
- E = Exercise and education
For patients being discharged home, emphasize the following:
- Timely follow-up with primary care provider
- Compliance with discharge medications, specifically aspirin and other medications used to control symptoms
- Need to return to the ED for any change in frequency or severity of symptoms
History
The severity and duration of coronary artery obstruction, the volume of myocardium affected, the level of demand, and the ability of the rest of the heart to compensate are major determinants of a patient's clinical presentation and outcome. A patient may present to the ED because of a change in pattern or severity of symptoms.
Typically, angina is a symptom of myocardial ischemia that appears in circumstances of increased oxygen demand. It is usually described as a sensation of chest pressure or heaviness that is reproduced by activities or conditions that increase myocardial oxygen demand. A new case of angina is more difficult to diagnose because symptoms are often vague and similar to those caused by other conditions (eg, indigestion, anxiety).
However, not all patients experience chest pain. They may present with only neck, jaw, ear, arm, or epigastric discomfort. Some patients, including some who are elderly or who have diabetes, present with no pain, complaining only of episodic shortness of breath, severe weakness, light-headedness, diaphoresis, or nausea and vomiting. Elderly persons may also present only with altered mental status. Those with preexisting altered mental status or dementia may have no recollection of recent symptoms and may have no complaints.
In addition, evidence exists that women more often have coronary events without typical symptoms, which may explain the frequent failure of clinicians to initially diagnose ACS in women.
A summary of patient complaints is as follows:
- Palpitations
- Pain, which is usually described as pressure, squeezing, or a burning sensation across the precordium and may radiate to the neck, shoulder, jaw, back, upper abdomen, or either arm
- Exertional dyspnea that resolves with pain or rest
- Diaphoresis from sympathetic discharge
- Nausea from vagal stimulation
- Decreased exercise tolerance
Stable angina involves episodic pain lasting 5-15 minutes, is provoked by exertion, and is relieved by rest or nitroglycerin. In unstable angina, patients have increased risk for adverse cardiac events, such as myocardial infarction or death. New-onset exertional angina can occur at rest and is of increasing frequency or duration or is refractory to nitroglycerin. Variant angina (Prinzmetal angina) occurs primarily at rest, is triggered by smoking, and is thought to be due to coronary vasospasm.
Physical Examination
Physical examination results are frequently normal. If chest pain is ongoing, the patient will usually lie quietly in bed and may appear anxious, diaphoretic, and pale. Physical findings can vary from normal to any of the following:
- Hypotension - Indicates ventricular dysfunction due to myocardial ischemia, infarction, or acute valvular dysfunction
- Hypertension - May precipitate angina or reflect elevated catecholamine levels due to anxiety or to exogenous sympathomimetic stimulation
- Diaphoresis
- Pulmonary edema and other signs of left heart failure
- Extracardiac vascular disease
- Jugular venous distention
- Cool, clammy skin and diaphoresis in patients with cardiogenic shock
In addition, a third heart sound (S3) may be present, and frequently, a fourth heart sound (S4) exists. The latter is especially prevalent in patients with inferior-wall ischemia and may be heard in patients with ischemia or systolic murmur secondary to mitral regurgitation
A systolic murmur related to dynamic obstruction of the left ventricular (LV) outflow tract may also occur. It is caused by hyperdynamic motion of the basal left ventricular myocardium and may be heard in patients with an apical infarct.
A new murmur may reflect papillary muscle dysfunction. Rales on pulmonary examination may suggest LV dysfunction or mitral regurgitation.
Patients who present to the ED with chest pain who have a low short-term risk of a major adverse cardiac event must be identified to facilitate early discharge in order to avoid lengthy and costly hospital stays. The ASPECT study tested a 2-hour, accelerated diagnostic protocol (ADP) that included the use of a structured pretest probability scoring method, electrocardiography, and a point-of-care biomarker panel that included troponin, creatine kinase MB, and myoglobin levels. The study suggests that ADP can identify patients at low risk for a short-term major adverse cardiac event who may be suitable for early discharge; such an approach could be used to decrease the overall observation periods and admissions for chest pain and has the potential to affect health-service delivery worldwide.
Complications
Complications of ischemia include pulmonary edema, while those of myocardial infarction include rupture of the papillary muscle, left ventricular free wall, and ventricular septum.
Work up
As previously mentioned, stable coronary artery disease (CAD) may result in ACS in the absence of plaque rupture and thrombosis, when physiologic stress (eg, trauma, blood loss, anemia, infection, tachyarrhythmias) increases demands on the heart. In such cases, the diagnosis of acute myocardial infarction can be made if workup reveals the typical rise and fall of biochemical markers of myocardial necrosis along with either the development of pathologic Q waves or the presence (on ECG or in the setting of a coronary intervention) of ischemic ST-segment changes. (However, the presence of ischemic symptoms can be substituted for the Q-wave or ST-segment evidence.)
Non–ST-segment elevation myocardial infarction (NSTEMI) is distinguished from unstable angina by elevated levels of cardiac enzymes and biomarkers of myocyte necrosis. Differentiation is generally based on 3 sets of biomarkers measured at 6- to 8-hour intervals after the patient's presentation to the ED. The current definition of NSTEMI requires a typical clinical syndrome plus elevated troponin (or creatine kinase isoenzyme MB [CK-MB]) levels to over 99% of the normal reference (with a coefficient of variation of < 10% for the assay). Given this definition, nearly 25% of patients who were previously classified as having unstable angina now fulfill the criteria for NSTEMI.
Measure cardiac enzyme levels at regular intervals, starting at admission and continuing until the peak is reached or until 3 sets of results are negative. Biochemical biomarkers (demonstrated in the image below) are useful for diagnosis and prognostication.
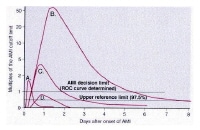 This plot shows changes in cardiac markers over time after the onset of symptoms. Peak A is the early release of myoglobin or creatine kinase isoenzyme MB (CK-MB) after acute myocardial infarction (AMI). Peak B is the cardiac troponin level after infarction. Peak C is the CK-MB level after infarction. Peak D is the cardiac troponin level after unstable angina. Data are plotted on a relative scale, where 1.0 is set at the myocardial-infarction cutoff concentration. Courtesy of Wu et al (1999). ROC = receiver operating characteristic.
This plot shows changes in cardiac markers over time after the onset of symptoms. Peak A is the early release of myoglobin or creatine kinase isoenzyme MB (CK-MB) after acute myocardial infarction (AMI). Peak B is the cardiac troponin level after infarction. Peak C is the CK-MB level after infarction. Peak D is the cardiac troponin level after unstable angina. Data are plotted on a relative scale, where 1.0 is set at the myocardial-infarction cutoff concentration. Courtesy of Wu et al (1999). ROC = receiver operating characteristic.
Of note, cardiac-specific troponins are not detectable in the blood of healthy individuals; therefore, they provide high specificity for detecting injury to cardiac myocytes. These molecules are also more sensitive than CK-MB for myocardial necrosis and therefore improve early detection of small myocardial infarctions. Although blood troponin levels increase simultaneously with CK-MB levels (about 6 h after the onset of infarction), they remain elevated for as long as 2 weeks. As a result, troponin values cannot be used to diagnose reinfarction. New methods of detecting troponins in the blood can measure levels as low as 0.1-0.2 ng/mL.
Keller et al suggest that among patients with suspected acute coronary syndrome, highly sensitive troponin I assay (hsTnI) or contemporary troponin I assay (cTnI) determination 3 hours after admission for chest pain may facilitate early rule-out of acute myocardial infarction. A serial change in hsTnI or cTnI levels from admission (using the 99th percentile diagnostic cutoff value) to 3 hours postadmission may aid in early diagnosis of acute myocardial infarction.
Minor elevations in these molecules can be detected in the blood of patients without ACS in the setting of myocarditis (pericarditis), sepsis, renal failure, acute congestive heart failure (CHF), acute pulmonary embolism, or prolonged tachyarrhythmias.
Guidelines released by the European Society of Cardiology (ESC) in August 2011 for the management of non-ST-segment elevation ACSs recommend GRACE or a similar scoring system to score the risk of an ischemic event in the short-to-mid term. The guidelines state that bleeding risk can be stratified using the CRUSADE (Can Rapid risk stratification of Unstable angina patients Suppress ADverse outcomes with Early implementation of the ACC/AHA guidelines) risk score.
Electrocardiography
ECGs should be reviewed promptly. Involve a cardiologist when in doubt.
Recording an ECG during an episode of the presenting symptoms is valuable. Transient ST-segment changes (>0.05 mV) that develop during a symptomatic period and that resolve when the symptoms do are strongly predictive of underlying CAD and have prognostic value. Comparison with previous ECGs is often helpful.
Alternative causes of ST-segment and T-wave changes are left ventricular aneurysm, pericarditis, Prinzmetal angina, early repolarization, Wolff-Parkinson-White syndrome, and drug therapy (eg, with tricyclic antidepressants, phenothiazines).
In the emergency setting, ECG is the most important ED diagnostic test for angina. It may show changes during symptoms and in response to treatment, confirm a cardiac basis for symptoms. It also may demonstrate preexisting structural or ischemic heart disease (left ventricular hypertrophy, Q waves). A normal ECG or one that remains unchanged from the baseline does not exclude the possibility that chest pain is ischemic in origin. Changes that may be seen during anginal episodes include the following:
- Transient ST-segment elevations
- Dynamic T-wave changes - Inversions, normalizations, or hyperacute changes
- ST depressions - May be junctional, downsloping, or horizontal
In patients with transient ST-segment elevations, consider LV aneurysm, pericarditis, Prinzmetal angina, early repolarization, and Wolff-Parkinson-White syndrome as possible diagnoses. Fixed changes suggest acute myocardial infarction.
When deep T-wave inversions are present, consider the possibility of central nervous system (CNS) events or drug therapy with tricyclic antidepressants or phenothiazines as the cause.
Diagnostic sensitivity may be increased by performing right-sided leads (V4 R), posterior leads (V8, V9), and serial recordings.
ECGs from 2 patients are shown below.
 A 50-year-old man with type 1 diabetes mellitus and hypertension presents after experiencing 1 hour of midsternal chest pain that began after eating a large meal. Pain is now present but is minimal. Aspirin is the single drug that will have the greatest potential impact on subsequent morbidity. In the setting of ongoing symptoms and electrocardiogram (ECG) changes, nitrates titrated to 10% reduction in blood pressure and symptoms, beta blockers, and heparin are all indicated. If the patient continues to have persistent signs and/or symptoms of ischemia, addition of a glycoprotein IIb/IIIa inhibitor should be considered.
A 50-year-old man with type 1 diabetes mellitus and hypertension presents after experiencing 1 hour of midsternal chest pain that began after eating a large meal. Pain is now present but is minimal. Aspirin is the single drug that will have the greatest potential impact on subsequent morbidity. In the setting of ongoing symptoms and electrocardiogram (ECG) changes, nitrates titrated to 10% reduction in blood pressure and symptoms, beta blockers, and heparin are all indicated. If the patient continues to have persistent signs and/or symptoms of ischemia, addition of a glycoprotein IIb/IIIa inhibitor should be considered. A 62-year-old woman with a history of chronic stable angina and a "valve problem" presents with new chest pain. She is symptomatic on arrival, complaining of shortness of breath and precordial chest tightness. Her initial vital signs are blood pressure = 140/90 mm Hg and heart rate = 98. Her electrocardiogram (ECG) is as shown. She is given nitroglycerin sublingually, and her pressure decreases to 80/palpation. Right ventricular ischemia should be considered in this patient.
A 62-year-old woman with a history of chronic stable angina and a "valve problem" presents with new chest pain. She is symptomatic on arrival, complaining of shortness of breath and precordial chest tightness. Her initial vital signs are blood pressure = 140/90 mm Hg and heart rate = 98. Her electrocardiogram (ECG) is as shown. She is given nitroglycerin sublingually, and her pressure decreases to 80/palpation. Right ventricular ischemia should be considered in this patient.
In difficult cases with nondiagnostic ECGs, such as those involving a left bundle-branch block, early imaging is useful to assess wall-motion abnormalities.
An important use of noninvasive imaging is to classify a patient has having NSTEMI or true STEMI.
The Optimal Cardiovascular Diagnostic Evaluation Enabling Faster Treatment of Myocardial Infarction (OCCULT-MI) trial compared the 80-lead (80L) mapping system to standard 12-lead (12L) ECG. The study concluded that the 80L body surface mapping technology detected more patients with MI or ACS than the 12L ECG, while still maintaining a high degree of specificity.
A study by Damman et al examined information from 5,420 patients from the Fragmin and Fast Revascularization During Instability in Coronary Artery Disease (FRISC II), Invasive Versus Conservative Treatment in Unstable Coronary Syndromes (ICTUS), and Randomized Intervention Trial of Unstable Angina 3 (RITA-3) patient-pooled database. The study found that admission ECG characteristics had long-term prognostic value for cardiovascular death or myocardial infarction. Quantitative ECG characteristics showed no incremental discrimination compared with qualitative data.
A 5-year follow-up of patients with non–ST-elevation acute coronary syndrome from these 3 trials found no link between a procedure-related MI and long-term cardiovascular mortality. However, long-term mortality substantially increased after a spontaneous MI.
Measurement of CK-MB Levels
CK-MB, the isoenzyme specific to the heart muscle, was the principal biomarker of cardiac injury until troponin supplemented it.
In the setting of myocardial infarction, plasma CK-MB concentrations typically rise about 4-6 hours after the onset of chest pain. They peak within 12-24 hours and return to baseline levels within 24-48 hours. Serial measurements obtained every 6-8 hours (at least 3 times) are warranted until peak values are determined.
The area under the concentration-time curve for CK-MB created with serial measurements of blood enzyme levels provides a reliable estimate of the size of the infarct.
Clinical settings other than ACS, such as trauma, heavy exertion, and skeletal muscle disease (eg, rhabdomyolysis), may elevate CK-MB values.
Determination of subforms of CK-MB (CK-MB2 that is more specific to heart muscle) may improve the sensitivity of this test.
Measurement of Troponin levels
The troponins are regulatory proteins found in skeletal and cardiac muscle. The 3 subunits that have been identified include troponin I (TnI), troponin T (TnT), and troponin C (TnC). The genes that code for the skeletal and cardiac isoforms of TnC are identical; thus, no structural difference exists between them. However, the skeletal and cardiac subforms for TnI and TnT are distinct, and immunoassays have been designed to differentiate between them. This explains the cardiospecificity of the cardiac troponins. Skeletal TnI and TnT are structurally different. No cross-reactivity occurs between skeletal and cardiac TnI and TnT with the current assays.
The cardiac troponins are sensitive, cardiospecific, and provide prognostic information for patients with ACS. They have become the cardiac markers of choice for patients with ACS.
Early studies on the release kinetics of the cardiac troponins indicated that they were not early markers of myocardial necrosis. The early generation troponin assays yielded positive results within 4-8 hours after symptom onset, similar in timing to the release of CK-MB; however, they remained elevated for as long as 7-10 days post-myocardial infarction.
Initial studies on the cardiac troponins revealed a subset of patients with rest unstable angina in whom CK-MB levels were normal but who had elevated troponin levels. These patients had higher adverse cardiac event rates (acute myocardial infarction, death) within the 30 days after the index admission and a natural history that closely resembled patients with NSTEMI. The table below outlines many of the initial studies on troponins in ACS.
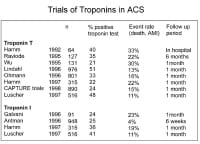 Use of cardiac markers in the ED. Studies on troponins in ACS.
Use of cardiac markers in the ED. Studies on troponins in ACS.
As previously mentioned, an elevated troponin level also enables risk stratification of patients with ACS and identifies patients at high risk for adverse cardiac events (ie, myocardial infarction, death) up to 6 months after the index event.
In a study by Antman et al, the initial TnI level on admission in patients with ACS correlated with mortality at 6 weeks. CK-MB levels, although sensitive and specific for the diagnosis of acute myocardial infarction, were not predictive of adverse cardiac events and had no prognostic value. The relationship between TnI levels and risk of cardiac events and mortality is demonstrated in the graphs below.
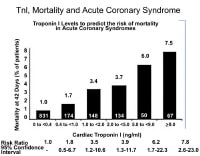 Use of cardiac markers in the ED. Troponin I levels and cardiac mortality in ACS.
Use of cardiac markers in the ED. Troponin I levels and cardiac mortality in ACS.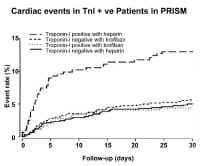 Use of cardiac markers in the ED. Cardiac event rates in the platelet receptor inhibition for ischemic syndrome (PRISM) study based on troponin I results.
Use of cardiac markers in the ED. Cardiac event rates in the platelet receptor inhibition for ischemic syndrome (PRISM) study based on troponin I results.
Data from a meta-analysis indicated that an elevated troponin level in patients without ST-segment elevation is associated with a nearly 4-fold increase in cardiac mortality rate. For the composite end point of acute myocardial infarction or death, an elevated troponin level was associated with an odds ratio of 3.3.
The TIMI IIIB, GUSTO IIa, GUSTO IV ACS, and Fragmin During Instability in Coronary Artery Disease (FRISC) trial all demonstrated a direct correlation between the level of TnI or TnT and the adverse cardiac event rate and mortality rate in ACS. These studies confirmed the use of the cardiac troponins TnI and TnT in risk stratification and therapeutic decision making.
Studies by Ohman et al and Stubbs et al revealed that an elevated troponin level at baseline was an independent predictor of mortality even in patients with chest pain and acute myocardial infarction with ST-segment elevation who were eligible for reperfusion therapy.
With the introduction of increasingly sensitive and precise troponin assays, up to 80% of patients with acute myocardial infarction will be found to have an elevated troponin within 2-3 hours of ED arrival. With this improved clinical performance in cardiac troponin assays, the so-called rapidly rising cardiac biomarkers, such as myoglobin or CK-MB isoforms, have little clinical utility. In a prospective multicenter study, patients with ACS who and presented with acute chest pain to the ED were followed for 12 months. The study found that patients with normal high-sensitivity cardiac troponin T (hs-cTnT) levels at presentation have low mortality rates but an increased rate of acute myocardial infarction during the subsequent 360 days.
As a result, some authorities have called for a troponin standard alone and recommend eliminating CK-MB.
Many patients with acute myocardial infarction present with equivocal ECG patterns, making prehospital ECG diagnosis difficult. A study by Sorensen et al suggests prehospital TnT testing may improve diagnosis in patients with chest pain transported by ambulance. When quantitative TnT was measured at hospital arrival in 958 patients after 8 and 24 hours, a diagnosis of acute myocardial infarction was established in 208 of 258 patients with increased TnT levels, showing prehospital TnT testing is feasible with a high success rate. Prehospital implementation of quantitative tests, with lower detection limits, may identify most patients with acute myocardial infarction irrespective of ECG changes.
The 2007 American College of Cardiology (ACC) guidelines for NSTEMI recommend that serial troponins be obtained for a definitive rule out at baseline and 6-9 hours later. To establish the diagnosis of acute myocardial infarction, only 1 elevated level above the established cutoff is required. The demonstration of a rising or falling level is needed to distinguish persistently elevated troponin levels (eg, in some patients with renal failure) from those patients with acute myocardial infarction.
If myocardial injury is suspected despite negative cardiac-specific troponin findings, additional, sensitive laboratory assays are indicated.
Patients with suspected ACS who test negative for troponin and copeptin can be safely discharged from the hospital without further testing, according to a recent study, the Biomarkers in Cardiology 8 (BiC-8) trial. Copeptin, a marker of severe hemodynamic stress, can be detected immediately in acute myocardial infarction. The study involved 902 patients at low to intermediate risk of ACS; half of the patients were treated with standard care, and the other 451 patients underwent a copeptin assay. In the latter group, patients with a positive copeptin test, defined as a level of 10 pmol/L or greater, were treated with standard ACS care, while patients with a copeptin level below 10 pmol/L were discharged into ambulant care, including an outpatient visit within 72 hours. In the 451 patients tested for troponin and treated with standard care, the 30-day rate of major adverse cardiovascular events was 5.5%, compared with 5.46% in the 451 patients tested for troponin and copeptin (a statisticallyinsignificant difference).
Measurement of Myoglobin Levels
Myoglobin is not cardiac specific, but it may be detected as early as 2 hours after myocardial necrosis starts. However, myoglobin results should be supplemented with other, more specific cardiac biomarkers, such as CK-MB or troponin.
Myoglobin values have a high negative predictive value when blood is sampled in the first 4-8 hours after onset.
Complete Blood Count Determination
The CBC count helps in ruling out anemia as a secondary cause of ACS. Leukocytosis has prognostic value in the setting of acute myocardial infarction.
Basic Metabolic Panel
Obtain a basic metabolic profile, including a check of blood glucose level, renal function, and electrolytes levels, for patients with new-onset angina. Close monitoring of potassium and magnesium levels is important in patients with ACS because low levels may predispose them to ventricular arrhythmias. Routine measurement of serum potassium levels and prompt correction are recommended.
Creatinine levels must be considered before using an angiotensin-converting enzyme (ACE) inhibitor and particularly if cardiac catheterization is considered. Use of N -acetylcysteine and adequate hydration can help prevent contrast material–induced nephropathy.
Other useful metabolic profiles include amylase and lipase.
A study by Charpentier et al suggests that a serum glucose level of more than 140 mg/dL is associated with non-ST elevation ACS in patients admitted to an ED for chest pain. However, when this level of blood glucose is added to the conventional diagnostic tools, the result is only a small increase in the ability to classify ACS.
New Biomarkers
levels of brain natriuretic peptide (BNP) and N-terminal pro-BNP (NT-pro-BNP) are elevated in acute MI and provide predictive information for risk stratification across the spectrum of ACS. However, a single, low BNP level obtained within 4 hours of a patient presenting to the ED does not identify the patient as low-risk for 30-day acute myocardial infarction or death.
In the future, a combination of levels of troponin (a biomarker for myocardial necrosis), NT-pro-BNP (an indicator of elevated LV end-diastolic pressure and wall stress), and C-reactive protein (CRP, an estimate of the extent of systemic inflammation) may prove useful for predicting the outcome of patients with ACS.
Routine measurement of BNP and CRP levels in patients with ACS is not warranted at this time.
Interleukin-6 is the major determinant of acute-phase reactant proteins in the liver, and serum amyloid A is another acute-phase reactant. Elevations of either of these can be predictive in determining increased risk of adverse outcomes in patients with unstable angina.
Cavusoqlu et al suggests that elevated baseline levels of plasma interleukin-10 are associated with long-term adverse outcomes in patients with ACS.
Several other biomarkers with variable sensitivity and specificity have been investigated, including sCD40 ligand, myeloperoxidase, pregnancy-associated plasma protein-A, choline, placental growth factor, cystatin C, fatty acid binding protein, ischemia modified albumin, chemokines ligand-5 and -18 (mediators of monocyte recruitment induced by ischemia), angiogenin, SCUBE1 (a novel platelet protein), and others. In a study that included 107 patients presenting to an emergency department with chest pain, ischemia modified albumin was not found to have superior sensitivity and specificity over traditional biomarkers, with a sensitivity of 0.86 and specificity of 0.49.
Chest Radiography
Chest radiography helps in assessing cardiomegaly and pulmonary edema, or it may reveal complications of ischemia, such as pulmonary edema. It may also provide clues to alternative causes of symptoms, such as thoracic aneurysm or pneumonia (which can be a precipitating cause of ACS).
Echocardiography
Echocardiograms may play an important role in the setting of ACS. Regional wall-motion abnormalities can be identified with this modality, and echocardiograms are especially helpful if the diagnosis is questionable.
An echocardiogram can also help in defining the extent of an infarction and in assessing overall function of the left and right ventricles. In addition, an echocardiogram can help to identify complications, such as acute mitral regurgitation, LV rupture, and pericardial effusion.
Absence of segmental wall-motion abnormality on echocardiography during active chest discomfort is a highly reliable indicator of a nonischemic origin of symptoms, although echocardiography is of limited value in patients whose symptoms have resolved or who have pre-existing wall-motion abnormalities.
Myocardial Perfusion Imaging
Radionuclide myocardial perfusion imaging has been shown to have favorable diagnostic and prognostic value in the emergent setting, with an excellent early sensitivity in the detection of acute myocardial infarction not found in other testing modalities.
A normal resting perfusion imaging study has been shown to have a negative predictive value of more than 99% in excluding myocardial infarction. Observational and randomized trials of rest and stress imaging in the ED evaluation of patients with chest pain have demonstrated reductions in unnecessary hospitalizations and cost savings compared with routine care.
Perfusion imaging has also been used in risk stratification after myocardial infarction and for measurement of infarct size to evaluate reperfusion therapies. Novel "hot spot" imaging radiopharmaceuticals that visualize infarction or ischemia are currently undergoing evaluation and hold promise for future imaging of ACS.
Cardiac Angiography
Cardiac catheterization helps in defining coronary anatomy and the extent of a patient’s disease.
Patients with cardiogenic shock, intractable angina (despite medication), severe pulmonary congestion, or right ventricular (RV) infarction should immediately undergo cardiac catheterization. (Cardiogenic shock is defined as a systolic BP of less than 90 mm Hg in the presence of organ hypoperfusion.)
For high-risk patients with ACS without persistent ST elevation, angiography with glycoprotein IIb/IIIa inhibition has been recommended. The earlier that coronary angiography is performed, the lower the risk of recurrent ischaemia. This also shortens the hospital stay for those patients.
Most patients benefit from angiography when they have a TIMI (Thrombolysis in Myocardial Infarction) risk score of less than 3 points (see the Table below).
Table. TIMI Risk Score for Unstable Angina and NSTEMI (Open Table in a new window)
| Characteristic | Risk Score |
| History | |
| Age ≥65 years | 1 |
| At least 3 risk factors for coronary heart disease | 1 |
| Previous coronary stenosis ≥50% | 1 |
| Use of aspirin in previous 7 days | 1 |
| Presentation | |
| At least 2 anginal episodes in the previous 24 hours | 1 |
| ST-segment elevation on admission ECG | 1 |
| Elevated levels of serum biomarkers | 1 |
| Total Score | 0-7 |
| Note: Event rates significantly increased as the TIMI risk score increased in the test cohort in the TIMI IIB study. Rates were 4.7% for a score of 0/1, 8.3% for 2, 13.2% for 3, 19.9% for 4, 26.2% for 5, and 40.9% for 6/7 (P < .001, χ2 test for the trend). The pattern of increasing event rates with increasing TIMI risk score was confirmed in all 3 validation groups (P < .001). | |
Computed Tomography Coronary Angiography and CT Coronary Artery Calcium Scoring
Dual-source 64-slice CT scanners can do a full scan in 10 seconds and produce high-resolution images that allow fine details of the patient's coronary arteries to be seen. This technology allows for noninvasive and early diagnosis of CAD and thus earlier treatment before the coronary arteries become more or completely occluded. It permits direct visualization of not only the lumen of the coronary arteries but also plaque within the artery. Dual-source 64-slice CT scanning is being used with intravenous (IV) contrast to determine if a stent or graft is open or closed.
CT coronary artery scoring is emerging as an attractive risk stratification tool in patients who are low risk for ACS. This imaging modality exposes the patient to very little radiation (1-2 msV). No contrast is needed, and the study does not have a requirement for heart rate.
The CAPTURE study, a randomized diagnostic trial, compared the efficacy a comprehensive cardiothoracic CT examination in the evaluation of patients presenting to the emergency department with undifferentiated acute chest discomfort or dyspnea. Comprehensive cardiothoracic CT scanning was reasonable, with a similar diagnostic yield to dedicated protocols, but it did not reduce the length of stay, rate of subsequent testing, or costs. The “triple rule out” protocol might be helpful in the evaluation of select patients, but these findings suggest that it should not be routinely used with the expectation that it will improve efficiency or reduce resource use.
Another study of the usefulness of CT for reducing hospital admission rates found that coronary computed tomographic angiography (CCTA) appears to allow safe, expedited discharge from the ED of low-to-intermediate-risk patients who would otherwise be admitted.
Other Techniques
Optical coherence tomography (OCT), palpography, and virtual histology are being studied for use in identifying vulnerable plaques.
Noninvasive whole-blood test prior to coronary angioplasty may be useful for assessing obstructive CAD in patients without diabetes.
Stress cardiac magnetic resonance imaging (MRI) in an observation unit setting has shown to reduce the medical costs, compared with inpatient care, for patients who present with emergent, non-low-risk chest pain, without missing acute coronary syndrome.
The CAPTURE study, a randomized diagnostic trial, compared the efficacy a comprehensive cardiothoracic CT examination in the evaluation of patients presenting to the emergency department with undifferentiated acute chest discomfort or dyspnea. Comprehensive cardiothoracic CT scanning was reasonable, with a similar diagnostic yield to dedicated protocols, but it did not reduce the length of stay, rate of subsequent testing, or costs. The “triple rule out” protocol might be helpful in the evaluation of select patients, but these findings suggest that it should not be routinely used with the expectation that it will improve efficiency or reduce resource use.
Treatment & Management
Initial therapy for acute coronary syndrome (ACS) should focus on stabilizing the patient's condition, relieving ischemic pain, and providing antithrombotic therapy to reduce myocardial damage and prevent further ischemia. Morphine (or fentanyl) for pain control, oxygen, sublingual or intravenous (IV) nitroglycerin, soluble aspirin 162-325 mg, and clopidogrel with a 300- to 600-mg loading dose are given as initial treatment.
In complete vessel occlusion without collateralization of the infarct-related vessel, there is little utility in “pushing nitrates.”
High-risk patients with non-ST-segment elevation myocardial infarction (NSTEMI ACS) should receive aggressive care, including aspirin, clopidogrel, unfractionated heparin or low–molecular-weight heparin (LMWH), IV platelet glycoprotein IIb/IIIa complex blockers (eg, tirofiban, eptifibatide), and a beta blocker. The goal is early revascularization.
Intermediate-risk patients with NSTEMI ACS should rapidly undergo diagnostic evaluation and further assessment to determine their appropriate risk category.
Low-risk patients with NSTEMI ACS should undergo further follow-up with biomarkers and clinical assessment. Optimal medical therapies include use of standard medical therapies, including beta blockers, aspirin, and unfractionated heparin or LMWH. The Clopidogrel in Unstable Angina to Prevent Recurrent Events (CURE) study showed that clopidogrel would be beneficial even in low-risk patients. If no further pain occurs, and follow-up studies are negative, a stress study should drive further management.
Monitor and immediately treat arrhythmias in the first 48 hours. Pay attention to exacerbating factors, such as disturbances in electrolytes (especially potassium and magnesium), hypoxemia, drugs, or acidosis. Correct these factors accordingly.
Humidified oxygen may reduce the risk of nosebleeds in patients with ACS who are receiving antiplatelet and antithrombin therapy.
Do not administer nitrates if the patient is hypotensive (systolic BP < 90 mm Hg); if RV infarction, large pericardial effusion, or severe aortic stenosis is suspected; or if the patient recently received phosphodiesterase-5 inhibitors (eg, sildenafil).
Patients with known hypersensitivity to antiplatelet agents, active internal bleeding, and bleeding disorders should not receive antiplatelet or antithrombotic therapy.
Some patients with intractable chest pain or severe hypotension may require the insertion of an intra-aortic balloon pump. The EuroHeart survey showed a nearly 40% reduction in the risk of death in patients with ACS who received support with an intra-aortic balloon pump. This benefit was independent of the status of the ST segment.
Congestive heart failure (CHF) can be due to systolic dysfunction or diastolic dysfunction in the setting of myocardial infarction. Aggressive treatment is indicated to prevent worsening of the situation.
Patients presenting with cardiogenic shock should undergo percutaneous coronary intervention (PCI) as soon as possible. Cardiogenic shock is associated with a high mortality rate. Pressor agents, such as dopamine, and inotropic agents, such as dobutamine, may be needed. In a prospective, natural-history study of coronary atherosclerosis, patients underwent 3-vessel coronary angiography and gray-scale and radiofrequency intravascular ultrasonographic imaging after PCI.
Recurrent ischemia may be due to incomplete reperfusion. In the setting of PCI, consider stent thrombosis as a possible cause. Whether drug-eluting stents have an increased rate of thrombosis compared with bare metal stents is unclear.
The clinical significance of incomplete coronary revascularization (ICR) following PCI in patients with ACS was examined in 2,954 patients from the Acute Catheterization and Urgent Intervention Triage Strategy (ACUITY) trial. At one year follow-up, ICR was strongly associated with ischemia-driven unplanned revascularization, myocardial infarction and major adverse cardiac events.
Drug-eluting stents are linked with fewer periprocedural risks but tend to have high incidence of postprocedural complications including myocardial infarction, repeat procedures, and 12-month major adverse cardiac and brain complications, compared with coronary bypass surgery.
One study by Ribichini et al suggests that prednisone treatment after bare metal stents or drug-eluting stent implantation results in a better event-free survival at 1 year.
In the final report of the HORIZONS-AMI trial, which assessed the 3 year outcomes of the effectiveness and safety of bivalirudin monotherapy and paclitaxel-eluting stenting, outcomes were sustained for patients with STEMI undergoing primary PCI.
In a study of 3031 patients, Mehta et al found that early intervention (coronary angiography < or = 24 h after randomization) in patients with ACS did not differ greatly from delayed intervention (coronary angiography > or = 36 h randomization) in the prevention of primary outcomes (ie, composite of death, myocardial infarction, or stroke at 6 mo). Early intervention did reduce the rate of secondary outcomes (ie, death, myocardial infarction, or refractory ischemia at 6 mo) and improved primary outcomes in patients who were at highest risk (ie, GRACE risk score >140).
In a Swedish registry of patients with STEMI from 1996-2007, reported an increase in the prevalence of evidence-based treatments. The use of aspirin, clopidogrel, beta blockers, statins, and ACE inhibitors all increased. Clopidogrel increased from 0% to 82%, statins increased from 23% to 83%, and various ACE inhibitors increased by a large margin. A decrease was reported in 30-day and 1-year mortality that was sustained during long-term follow-up. By following the proper guidelines, patients who have experienced STEMI have higher survival rates.
Pharmacologic Anti-ischemic Therapy
Nitrates
Nitrates do not improve mortality. However, they provide symptomatic relief by means of several mechanisms, including coronary vasodilation, improved collateral blood flow, decrease in preload (venodilation and reduced venous return), and decrease in afterload (arterial vasodilation). Care should be taken to avoid hypotension, because this can potentially reduce coronary perfusion pressure (diastolic BP - LV diastolic pressure).
Beta-blockers
Beta-blockers are indicated in all patients unless they have the following contraindications:
- Systolic blood pressure less than 90 mm Hg
- Cardiogenic shock
- Severe bradycardia
- Second- or third-degree heart block
- Asthma or emphysema that is sensitive to beta agonists
- Peripheral vascular disease
- Uncompensated CHF
Beta blockers reduce oxygen demand and ventricular wall tension. They also decrease mortality and adverse cardiovascular events. These drugs may prevent mechanical complications of myocardial infarction, including rupture of the papillary muscle, left ventricular free wall, and ventricular septum. Beta blockers meliorate dynamic obstruction of the left ventricular outflow tract in patients with apical infarct and hyperdynamic basal segments.
The most frequently used regimen is IV metoprolol 2-5 mg given every 5 minutes (up to 15 mg total) followed by 25-100 mg given orally twice a day.
Beta-blockers should not be used acutely in patients with cardiogenic shock or signs of heart failure on presentation.
Pharmacologic Antithrombotic Therapy
Aspirin
Aspirin permanently impairs the cyclooxygenase pathway of thromboxane A2 production in platelets, in this way inhibiting platelet function. Aspirin reduces morbidity and mortality and is continued indefinitely.
Clopidogrel
Clopidogrel (thienopyridine) inhibits adenosine 5'-diphosphate (ADP)–dependent activation of the glycoprotein IIb/IIIa complex, a necessary step for platelet aggregation. This process results in intense inhibition of platelet function, particularly in combination with aspirin. In the CURE trial, thienopyridine reduced the rate of myocardial infarction by 20%.
Clopidogrel is a class I recommendation for patients when an early noninterventional approach is planned in therapy for at least 1 month and ideally up to 1 year. When percutaneous coronary intervention (PCI) is planned, clopidogrel 300-600 mg should be given as early as possible before or at the time of PCI. Clopidogrel, 75 mg daily, is continued for at least 12 months after PCI, if the patient is not at high risk for bleeding, according to 2011 ACCF/AHA guidelines (class I recommendation). Early discontinuation should be considered if the risk of bleeding-related morbidity outweighs the anticipated benefits.
The optimal loading dose for clopidogrel is still being evaluated. Reports show that a loading dose of 600 mg might be more beneficial than 300 mg. Withhold clopidogrel for at least 5 days before elective coronary artery bypass grafting (CABG). Since 12% of patients with non-ST elevation ACS have coronary anatomy that favors CABG, the use of clopidogrel is withheld until coronary angiography at some institutions.
A meta-analysis of 34 studies analyzed the safety of CABG among patients with ACS continuing clopidogrel. The investigators found that although mortality is increased in those receiving clopidogrel, it is influenced by ACS status and case urgency in primarily nonrandomized studies. Among patients with ACS, no differences in mortality or postoperative myocardial infarction or stroke rates were found. This suggests that in patients with ACS who require urgent CABG, proceeding despite the continuation of clopidogrel is likely safe.
Clopidogrel can be considered an alternative to aspirin in patients with aspirin intolerance or who are allergic to aspirin.
Patients with chronic kidney disease who have low platelet response to clopidogrel tend to have worse outcomes after PCI.
A consensus statement issued by the American College of Cardiology, American College of Gastroenterology, and American Heart Association in November 2010 addresses the issue of concomitant use of proton pump inhibitors (PPIs) and thienopyridine antiplatelet drugs.
Evidence has shown that dexlansoprazole and lansoprazole do not significantly reduce the conversion of clopidogrel to its active metabolite (reduced by 9% and 14%, respectively), and no dose adjustment of clopidogrel is required.
The group’s findings and recommendations are listed below.
- Clopidogrel reduces major CV events compared with placebo or aspirin.
- Dual antiplatelet therapy with clopidogrel and aspirin, compared with aspirin alone, reduces major CV events in patients with established ischemic heart disease, and it reduces coronary stent thrombosis but is not routinely recommended for patients with prior ischemic stroke because of the risk of bleeding.
- Clopidogrel alone, aspirin alone, and their combination are all associated with increased risk of GI bleeding.
- Clopidogrel requires metabolic activation by cytochrome P450 2C19 (CYP2C19). PPIs that inhibit CYP2C19 are commonly coadministered with clopidogrel to reduce the risk of GI bleeding. A study by Simon et al showed that PPI use is not associated with an increased risk of cardiovascular events or mortality in patients who have been treated with clopidogrel for a recent MI, regardless of CYP2C19 genotype.
- Patients with prior GI bleeding are at highest risk for recurrent bleeding on antiplatelet therapy; other risk factors include advanced age, concurrent use of anticoagulants, steroids, or NSAIDs including aspirin, and Helicobacter pyloriinfection; risk increases as the number of risk factors increases.
- Use of PPIs or histamine H2 receptor antagonists (H2RAs) reduces the risk of upper GI bleeding compared with no therapy; PPIs reduce upper GI bleeding to a greater degree than do H2Ras.
- PPIs are recommended to reduce GI bleeding among patients with a history of upper GI bleeding; PPIs are appropriate in patients with multiple risk factors for GI bleeding who require antiplatelet therapy.
- Routine use of either a PPI or an H2RA is not recommended for patients at lower risk of upper GI bleeding, who have much less potential to benefit from prophylactic therapy.
- Clinical decisions regarding concomitant use of PPIs and thienopyridines must balance overall risks and benefits, considering both CV and GI complications.
- Pharmacokinetic and pharmacodynamic studies, using platelet assays as surrogate endpoints, suggest that concomitant use of clopidogrel and a PPI reduces the antiplatelet effects of clopidogrel; the strongest evidence for an interaction is between omeprazole and clopidogrel; it is not established that changes in these surrogate endpoints translate into clinically meaningful differences.
- Observational studies and a single randomized clinical trial have shown inconsistent effects on CV outcomes of concomitant use of thienopyridines and PPIs; a clinically important interaction cannot be excluded, particularly in certain subgroups, such as poor metabolizers of clopidogrel.
- The role of either pharmacogenomic testing or platelet function testing in managing therapy with thienopyridines and PPIs has not yet been established.
Prasugrel
Like clopidogrel, prasugrel is a thienopyridine ADP receptor inhibitor that inhibits platelet aggregation. It has been approved in the United States and has been shown to reduce new and recurrent myocardial infarctions. The loading dose is 60 mg PO once and maintenance is 10 mg PO qd (given with aspirin 75-325 mg/d). Prasugrel is indicated for the reduction of thrombotic cardiovascular events (including stent thrombosis) with ACS that is managed with PCI.
The 2011 ACF/AHA guidelines advise that a loading dose of prasugrel be given as soon as possible, once coronary anatomy is defined and a decision is made to proceed with PCI. Prasugrel should be administered no later than 1 hour after PCI. Maintenance therapy with prasugrel is continued for at least 1 year after PCI. Early discontinuation should be considered if the risk of bleeding-related morbidity outweighs the anticipated benefits.
However, a 2014 report by Montalescot et al indicates that if angiography is to be performed in a patient with NSTEMI within 48 hours of admission, treatment with the P2Y12 antagonist prasugrel should be postponed until a decision about revascularization has been reached owing to an increased bleeding risk without ischemia benefit from pre-PCI prasugrel therapy. The randomized, double-blind study included 2770 NSTEMI patients who underwent percutaneous coronary intervention (PCI), with 1394 patients receiving pretreatment with prasugrel and 1376 individuals receiving placebo. All patients received prasugrel at the time of PCI.
The investigators found that the same percentage of patients (13.1%) in the pretreatment and placebo groups reached primary endpoint (defined as time to first occurrence of glycoprotein IIb/IIIa bailout, stroke, myocardial infarction [MI], urgent revascularization, or cardiovascular death, through 7 days after randomization). No reductions in ischemic events, including total mortality, were found in the patients who received prasugrel pretreatment. Moreover, pretreatment with prasugrel was associated with a six-fold increase in life-threatening bleeding unrelated to coronary artery bypass grafting (CABG), as well as a three-fold increase in all major bleeding associated with non-CABG thrombolysis in myocardial infarction (TIMI). An approximately three-fold increase in TIMI minor bleeding events was also seen.
Earlier studies also found that significant, sometimes fatal, bleeding occurred more frequently with prasugrel than with clopidogrel, although the overall mortality rate did not differ significantly between a treatment group receiving prasugrel and another receiving clopidogrel.
In a separate, earlier study of patients with unstable angina or myocardial infarction without ST-segment elevation, prasugrel, compared with clopidogrel, did not significantly reduce the frequency of the primary end point of death from cardiovascular causes, myocardial infarction, or stroke. Similar bleeding risks were observed.
Vorapaxar
In May 2014, the FDA approved vorapaxar (Zontivity) to reduce the risk of MI, stroke, cardiovascular death, and need for revascularization procedures in patients with a previous MI or peripheral artery disease (PAD). It is a first-in-class antiplatelet medication that is a protease-activated receptor 1 (PAR-1) inhibitor. It is not indicated as monotherapy, but in addition to aspirin and/or clopidogrel.
Approval was based on the Thrombin-Receptor Antagonist in Secondary Prevention of Atherothrombotic Ischemic Events (TRA 2°P TIMI-50) trial. Results of the trial (n = 26,499) showed that time to cardiovascular death, MI, stroke, or urgent coronary revascularization was decreased by 13% in patients taking vorapaxar. When coronary revascularization was excluded, the secondary endpoint of cardiovascular death, MI, or stroke was also significantly reduced.
Because of vorapaxar’s antiplatelet effects, moderate or severe bleeding occurred in 3.4% of patients compared with 2.1% in the placebo-treated patients. Intracranial hemorrhage occurred in 0.6% of those taking vorapaxar compared with 0.4% taking placebo.
Ticagrelor
Ticagrelor (Brilinta) was approved by the US Food and Drug Administration in July 2011 and is the first reversible oral P2Y receptor antagonist. Results from the randomized PLATO (PLATelet inhibition and patient Outcomes) trial showed that ticagrelor provides faster, greater, and more consistent ADP-receptor inhibition than clopidogrel.
In the PLATO trial, the difference between treatments on the composite resulted from effects on CV death and MI; each was statistically significant when considered as a secondary endpoint, and there was no beneficial effect on strokes. For all-cause mortality, the benefit was also statistically significant of 9.8% for ticagrelor and 11.7% for clopidogrel (p = 0.0003) with a hazard ratio of 0.78.
Bleeding risk was assessed in the PLATO trial, and ticagrelor increased the overall risk of bleeding (major + minor) to a somewhat greater extent than did clopidogrel. The increase was seen for non-CABG-related bleeding but not for CABG-related bleeding. Fatal and life-threatening bleeding rates were not increased.
Prevention of stent thrombosis
A subgroup analysis of the PLATO trial indicated that treatment with ticagrelor resulted in a lower risk of stent thrombosis than treatment with clopidogrel in patients with ACS. This benefit was independent of patient characteristics at baseline, including type of ACS and stent type.
Of the 18,624 ACS patients in the PLATO study, 11,289 (61%) had a previous stent implanted or received one during the trial. Of these, 177 patients (1.6%) had a definite stent thrombosis (176 of them within 1 year), and 275 (2.5%) had definite or probable stent thrombosis.
Definite stent thrombosis occurred in 1.37% of patients treated with ticagrelor and 1.93% of those treated with clopidogrel—a 33% reduction in risk with ticagrelor. Definite or probable stent thrombosis occurred in 2.21% of ticagrelor-treated patients and 2.87% of those who received clopidogrel—a 25% reduction in risk with ticagrelor. Overall, the risk of definite, probable, or possible stent thrombosis was reduced by 23% with ticagrelor.
Abciximab, eptifibatide, and tirofiban
Glycoprotein IIb/IIIa receptor antagonists include abciximab, eptifibatide, and tirofiban. These drugs inhibit the glycoprotein IIb/IIIa receptor, which is involved in the final common pathway for platelet adhesion and aggregation. (See the image below.)
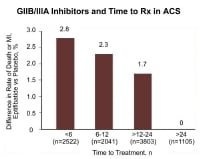 Use of cardiac markers in the ED. Effect of time to treatment in patients with acute coronary syndrome (ACS) who are treated with the GIIb/IIIa inhibitor eptifibatide.
Use of cardiac markers in the ED. Effect of time to treatment in patients with acute coronary syndrome (ACS) who are treated with the GIIb/IIIa inhibitor eptifibatide.
Use eptifibatide or tirofiban in patients with high-risk features in whom invasive treatment is not planned.
The use of eptifibatide 12 hours or more before angiography was not superior to the provisional use of eptifibatide after angiography, according to results from the EARLY ACS trial. The study compared a strategy of early, routine administration of eptifibatide with delayed, provisional administration in patients who had ACS without ST-segment elevation and who were assigned to an invasive strategy. The study also found that early use of eptifibatide was associated with an increased risk of non–life-threatening bleeding and the need for transfusion.
Two trials with tirofiban and 1 trial with eptifibatide documented their efficacy in unstable angina/NSTEMI patients, only some of whom underwent interventions. These antagonists are a class I recommendation in patients in whom catheterization and PCI are planned. Intermediate- and high-risk patients appear to respond favorably to glycoprotein IIb/IIIa inhibitors. They include patients with ST-segment depression, elevated risk scores, elevated serum troponin levels, and/or diabetes mellitus.
Currently, IIb/IIIb antagonists in combination with aspirin are considered standard antiplatelet therapy for patients at high risk for unstable angina.
Pharmacologic Anticoagulation Therapy
Unfractionated heparin
A study by Oler et al found that unfractionated heparin was associated with a 33% reduction in the risk of myocardial infarction or death in patients with unstable angina who were treated with aspirin plus heparin, compared with patients who were treated with aspirin alone. The FUTURA/OASIS-8 randomized trial found that low-dose unfractionated heparin, 50 U/kg (regardless of use of glycoprotein IIb/IIIa inhibitors), compared with standard-dose unfractionated heparin, 85 U/kg (60 U/kg with Gp IIb/IIIa inhibitors), did not reduce major peri-PCI bleeding and vascular access-site complications.
Low–molecular-weight heparin
LMWHs might be superior to unfractionated heparin in reducing cardiovascular outcomes, with a safety profile similar to that of heparin in patients receiving medical care.
Conflicting results emerged from 9 randomized trials directly comparing LMWH with unfractionated heparin. Two trials evaluated dalteparin, another evaluated nadroparin, and 6 evaluated enoxaparin. Trials with dalteparin and nadroparin reported similar rates of nonfatal myocardial infarction or death compared with heparin, whereas 5 of 6 trials of enoxaparin found point estimates for death or nonfatal myocardial infarction that favored enoxaparin over heparin. The benefit of enoxaparin appeared to be driven largely by a reduction in nonfatal myocardial infarction, especially in the cohort of patients who had not received any open-label anticoagulant therapy before randomization.
In addition, a systematic review comparing LMWH with unfractionated heparin found no significant difference in benefits between the 2 drugs.
Aside from the possible medical benefits of using LMWH in place of unfractionated heparin, advantages of LMWH include ease of administration, absence of need for anticoagulation monitoring, and potential for overall cost savings. Although 3 LMWHs are approved for use in the United States, only enoxaparin is currently approved for use in unstable angina. Lev et al found that the combination of eptifibatide with enoxaparin appears to have a more potent antithrombotic effect than that of eptifibatide and unfractionated heparin.
The role of LMWHs in patients for whom PCI is scheduled is relatively ill defined. However, it is likely to be at least equivalent to that of heparin. It appears reasonable to minimize the risk of excessive anticoagulation during PCI by avoiding crossover of anticoagulants (ie, maintain consistent anticoagulant therapy from the pre-PCI phase throughout the procedure itself). Additional experience with regard to the safety and efficacy of the concomitant administration of LMWHs with Gp IIb/IIIa antagonists and fibrinolytic agents is currently being acquired.
Adding apixaban (5 mg twice daily) to antiplatelet therapy in high-risk patients after ACS may increase the number of major bleeding events without significantly reducing recurrent ischemic events.
Factor Xa inhibitors
Use of the oral Xa inhibitor rivaroxaban in patients with ACS was investigated in the ATLAS ACS 2-TIMI 51 trial. Cutting the rivaroxaban dosage from 5 mg twice daily to 2.5 mg twice daily reduced deaths and bleeding after ACS. Mortality from recurrent events was significantly lower with the 2.5-mg dose (30.6% vs 43.8%), as was the death rate from new MI (8.8% vs 17.2%). The risk of fatal bleeding was 61% lower with the 2.5-mg dose, and rates of TIMI bleeding requiring medical attention were significantly lower (12.9% vs 16.2%).
Another factor Xda inhibitor, fondaparinux (Arixtra), has been studied for use in patients with STEMI who do not undergo PCI. In the Fifth Organization to Assess Strategies in Ischemic Syndromes (OASIS-5) trial, fondaparinux reduced major bleeding and improved net clinical outcome compared with enoxaparin in patients receiving GP IIb/IIIa inhibitors or thienopyridines for ACS. Fondaparinux is not currently FDA approved for use in ACS.
Thrombolysis
Prehospital thrombolysis allows eligible patients to receive thrombolysis 30-60 minutes sooner than if treatment were given in the ED; however, prehospital thrombolysis is still under investigation and has not become a trend, as a result of unproven benefit and an increase in the availability of PCI in many medical centers as an alternative to thrombolysis for STEMI.
The Remodeling With Erythropoietin After Large Myocardial Infarction (REVEAL) trial evaluated the safety and efficacy of a single intravenous bolus of epoetin alfa in patients with STEMI who had successful reperfusion with primary or rescue PCI. A single intravenous bolus of epoetin alfa within 4 hours of PCI did not reduce infarct size and was associated with higher rates of adverse cardiovascular events.
Although PCI is the preferred treatment for STEMI, the distance to primary PCI centers and the inherent time delay in delivering primary PCI limits widespread use of this treatment. Prehospital electrocardiographic (ECG) diagnosis and direct referral for primary PCI enables patients with STEMI living far from a PCI center to achieve a system delay comparable to patients who are closer to a PCI center.
Coronary Interventions
An early invasive strategy (ie, diagnostic angiography with intent to perform revascularization) is indicated in unstable angina/NSTEMI patients who have refractory angina or hemodynamic or electrical instability without serious comorbidities or contraindications to such procedures. An early invasive strategy is also indicated in initially stabilized unstable angina/NSTEMI patients who do not have serious comorbidities or contraindications to such procedures and who have an elevated risk for clinical events.
According to the 2011 American College of Cardiology Foundation/American Heart Association (ACCF/AHA) guidelines, an early invasive strategy (ie, within 12-24 hours of admission) is a reasonable choice for initially stabilized high-risk patients with unstable angina/NSTEMI; for patients not at high risk , a delayed invasive approach is also reasonable (class IIa recommendation).
In NSTEMI ACS, early revascularization reduces myocardial infarction and death rates compared with a more selective strategy, particularly in high-risk patients. Use of Gp IIb/IIIa blockers followed by early invasive catheterization is the most logical approach. An early invasive strategy should be considered in patients with large myocardial infarction, hypotension, shock, RV infarction, and refractory chest pain.
In the Invasive Versus Conservative Treatment in Unstable Coronary Syndromes (ICTUS) trial, an early invasive strategy had no apparent long-term benefit in reducing death or myocardial infarction. After stratification for risk, analysis of 5-year clinical outcomes in patients presenting with non-ST-segment elevation ACS and elevated troponin T (TnT) level showed that cumulative myocardial infarction or death rates were 22.3% in the early invasive group versus 18.1% in the selective invasive group. No difference was observed in mortality or myocardial infarction.
Concomitant Therapy
Current guidelines for patients with moderate- or high-risk ACS recommend an early invasive approach with concomitant antithrombotic therapy, including aspirin, clopidogrel, and unfractionated or LMWH. The Acute Catheterization and Urgent Intervention Triage Strategy (ACUITY) trial evaluated the role of thrombin-specific anticoagulation with bivalirudin in this patient population. In patients with moderate- or high-risk ACS who were undergoing invasive treatment with glycoprotein IIb/IIIa inhibitors, bivalirudin was associated with rates of ischemia and bleeding that were similar to those with heparin. Bivalirudin alone was associated with similar rates of ischemia and significantly lower rates of bleeding. Further, glycoprotein IIb/IIIa inhibitors can be initiated at the time of angiography; routine administration 12-24 hours before the procedure carries an increased risk of bleeding and no improvement in outcome.
Kastrati et al compared the combination of glycoprotein IIb/IIIa inhibitors and heparin with bivalirudin, specifically among patients with NSTEMI undergoing PCI. In a double-blind manner, 1721 patients with acute NSTEMI were randomly assigned to receive abciximab plus unfractionated heparin (861 patients) or bivalirudin (860 patients). The study concluded that abciximab and unfractionated heparin, compared with bivalirudin, failed to reduce death, large recurrent myocardial infarction, urgent target-vessel revascularization, or major bleeding within 30 days. It also increased the risk of bleeding among patients with NSTEMI who were undergoing PCI.
Medication Summary
The goals of treatment are to preserve patency of the coronary artery, augment blood flow through stenotic lesions, and reduce myocardial oxygen demand. All patients should receive antiplatelet agents, and patients with evidence of ongoing ischemia should receive aggressive medical intervention until signs of ischemia, as determined by symptoms and ECG, resolve.
Antiplatelet agents
Class Summary
Antiplatelets inhibit the cyclooxygenase system, decreasing the level of thromboxane A2, which is a potent platelet activator. Antiplatelet therapy reduces mortality by reducing the risk of fatal strokes and fatal myocardial infarctions.
Aspirin (Anacin, Ascriptin, Bayer Aspirin)
Early administration of aspirin (eg, Anacin, Ascriptin, Bayer Aspirin) in patients with acute myocardial infarction may reduce cardiac mortality in the first month. The adult dose is 160-324 mg PO or chewed. It can be administered as a suppository if the patient is unable to take PO medications. Aspirin reduces morbidity and mortality and is continued indefinitely. If administered with ticagrelor (Brilinta), do not exceed 100 mg/day after a one-time loading dose of 325 mg.
Vorapaxar (Zontivity)
Vorapaxar reversibly inhibits protease-activated receptor 1 (PAR-1) which is expressed on platelets, but its long half-life makes it effectively irreversible. It is indicated to reduce thrombotic cardiovascular events in patients with a history of MI or with peripheral arterial disease. It is not used as monotherapy, but added to aspirin and/or clopidogrel.
Nitrates
Class Summary
Nitrates oppose coronary artery spasm and reduce myocardial oxygen demand by reducing preload and afterload.
Nitroglycerin topical (Nitro-Bid)
Nitroglycerin (Nitro-Bid) causes relaxation of the vascular smooth muscle via stimulation of intracellular cyclic guanosine monophosphate production, causing a decrease in blood pressure. Nitrates do not improve mortality. However, they provide symptomatic relief by means of several mechanisms, including coronary vasodilation, improved collateral blood flow, decrease in preload (venodilation and reduced venous return), and decrease in afterload (arterial vasodilation). Care should be taken to avoid hypotension, because this can potentially reduce coronary perfusion pressure (diastolic BP - LV diastolic pressure).
Analgesics
Class Summary
These agents reduce pain which decreases sympathetic stress, in addition to providing some preload reduction.
Morphine sulfate (Duramorph, Astramorph, MS Contin)
Morphine sulfate (Duramorph, Astramorph, MS Contin) is the drug of choice for narcotic analgesia because of its reliable and predictable effects, safety profile, and ease of reversibility with naloxone. Morphine sulfate administered intravenously may be dosed in a number of ways and commonly titrated until the desired effect is obtained.
Beta-adrenergic blockers
Class Summary
Beta blockers have antiarrhythmic and antihypertensive properties, as well as the ability to reduce ischemia. They minimize the imbalance between myocardial supply and demand by reducing afterload and wall stress. In patients with acute MI, they decrease infarct size as well as short- and long-term mortality, which is a function of their anti-ischemic and antiarrhythmic properties. These drugs may prevent mechanical complications of myocardial infarction, including rupture of the papillary muscle, left ventricular free wall, and ventricular septum. Beta blockers ameliorate dynamic obstruction of the left ventricular outflow tract in patients with apical infarct and hyperdynamic basal segments. They should not be used acutely in patients with cardiogenic shock or signs of heart failure on presentation.
Metoprolol (Lopressor)
Metoprolol (Lopressor) is a selective beta1-adrenergic receptor blocker that decreases the automaticity of contractions. During IV administration, blood pressure, heart rate, and ECG should be carefully monitored. The goal of treatment is to reduce the patient's heart rate to 60-90 beats/min.
Esmolol (Brevibloc)
Esmolol (Brevibloc) is an excellent drug for use in patients at risk for complications from beta blockers, particularly reactive airway disease, mild to moderate LV dysfunction, and peripheral vascular disease. Its short half-life of 8 min allows for titration to desired effect with the ability to stop quickly prn.
Glycoprotein IIB/IIIA inhibitors
Class Summary
Glycoprotein IIb/IIIa receptor antagonists include abciximab, eptifibatide, and tirofiban. Glycoprotein IIb/IIIa antagonists prevent the binding of fibrinogen, thereby blocking platelet aggregation. These drugs inhibit the glycoprotein IIb/IIIa receptor, which is involved in the final common pathway for platelet adhesion and aggregation. Currently, GP IIb/IIIb receptor antagonists in combination with aspirin are considered standard antiplatelet therapy for patients at high risk for unstable angina.
Abciximab (ReoPro)
Abciximab (ReoPro) is a chimeric human-murine monoclonal antibody. It binds to receptors with high affinity and reduces platelet aggregation by 80%. Inhibition of platelet aggregation persists for up to 48 hours after the end of infusion. Abciximab has been approved for use in elective/urgent/emergent percutaneous coronary intervention.
Eptifibatide (Integrilin)
Eptifibatide (Integrilin) is an antagonist of the platelet GP IIb/IIIa receptor; it reversibly prevents von Willebrand factor, fibrinogen, and other adhesion ligands from binding to the GP IIb/IIIa receptor. The end effect is the inhibition of platelet aggregation. The effects persist over the duration of maintenance infusion and are reversed when infusion ends. Use eptifibatide (or tirofiban, see below) in patients with high-risk features in whom invasive treatment is not planned.
Tirofiban (Aggrastat)
Tirofiban (Aggrastat) is a nonpeptide antagonist of the GP IIb/IIIa receptor. It is a reversible antagonist of fibrinogen binding. When administered intravenously, more than 90% of platelet aggregation is inhibited. Tirofiban has been approved to reduce the rate of thrombotic cardiovascular events (combined endpoint of death, myocardial infarction, or refractory ischemia/repeat cardiac procedure) in patients with non-ST elevation acute coronary syndrome (NSTE-ACS).
Anticoagulants
Class Summary
Anticoagulants are used to prevent recurrence of clot after a spontaneous fibrinolysis.
Heparin
Heparin augments the activity of antithrombin III and prevents the conversion of fibrinogen to fibrin. It does not actively lyse but is able to inhibit further thrombogenesis. This agent prevents recurrence of a clot after spontaneous fibrinolysis.
Low molecular weight heparins
Class Summary
LMWH is indicated for treatment of ST-segment elevation myocardial infarction (STEMI) managed medically or with subsequent PCI. It is also indicated as prophylaxis for ischemic complications caused by unstable angina and non–Q-wave myocardial infarction.
Aside from the possible medical benefits of using LMWH in place of unfractionated heparin, advantages of LMWH include ease of administration, absence of need for anticoagulation monitoring, and potential for overall cost savings. Although 3 LMWHs are approved for use in the United States, only enoxaparin is currently approved for use in unstable angina.
Enoxaparin (Lovenox)
Low-molecular-weight heparin (enoxaparin; Lovenox), which is produced by partial chemical or enzymatic depolymerization of unfractionated heparin, binds to antithrombin III, enhancing its therapeutic effect. The heparin–antithrombin III complex binds to and inactivates activated factor X (Xa) and factor II (thrombin). LMWH differs from unfractionated heparin by having a higher ratio of antifactor Xa to antifactor IIa than does unfractionated heparin. Maximum antifactor Xa and antithrombin activities occur 3-5 hours after administration.
Direct thrombin inhibitors
Class Summary
Direct thrombin inhibitors bind directly to the anion binding site and the catalytic sites of thrombin to produce potent and predictable anticoagulation.
Hirudin (Lepirudin, Refludan)
Hirudin (Lepirudin, Refludan) is the prototype of direct thrombin inhibitors. Hirudin binds directly to the anion binding site and the catalytic sites of thrombin to produce potent and predictable anticoagulation. Currently, hirudin is indicated only in patients who are unable to receive heparin because of heparin-induced thrombocytopenia.
Bivalirudin (Angiomax)
Bivalirudin (Angiomax) is a synthetic analogue of recombinant hirudin. It inhibits thrombin and is used for anticoagulation in unstable angina in patients undergoing PTCA. Potential advantages over conventional heparin therapy include more predictable and precise levels of anticoagulation, activity against clot-bound thrombin, absence of natural inhibitors (eg, platelet factor 4, heparinase), and continued efficacy following clearance from plasma (because of binding to thrombin).
Adenosine diphosphate receptor antagonists
Class Summary
Thienopyridine adenosine 5'-diphosphate (ADP) antagonists approved for antiplatelet activity in the United States include clopidogrel, ticlopidine, prasugrel, and ticagrelor. All but ticagrelor have irreversible antiplatelet activity and take several days to manifest an effect, whereas, ticagrelor is a reversible P2Y12 receptor inhibitor. A potential additive benefit exists when ADP antagonists are used in conjunction with aspirin. These drugs may be considered alternatives to aspirin in patients with aspirin intolerance or who are allergic to aspirin.
Clopidogrel (Plavix)
Clopidogrel (Plavix) inhibits ADP-dependent activation of the glycoprotein IIb/IIIa complex, a necessary step for platelet aggregation. This process results in intense inhibition of platelet function, particularly in combination with aspirin.
Clopidogrel can be considered an alternative to aspirin in patients with aspirin intolerance or who are allergic to aspirin. The CURRENT-OASIS 7 trial suggests that a 7-day double-dose clopidogrel regimen can be considered for patients with acute coronary syndromes, as the efficacy and safety did not differ from that of a high- and low-dose aspirin regimen. However, there is no benefit in the double-dose treatment for patients who are undergoing an early invasive strategy.
Clopidogrel is a class I recommendation for patients when an early noninterventional approach is planned in therapy. When percutaneous coronary intervention (PCI) is planned, clopidogrel is started and continued for at least 1 month and for up to 9 months, if the patient is not at high risk for bleeding.
Clopidogrel is generally preferred over ticlopidine (Ticlid), because it more rapidly inhibits platelets and appears to have a more favorable safety profile.
Clopidogrel has been suggested to be less effective in reducing the rate of cardiovascular events in individuals who carry the loss-of-function CYP2C19 alleles. However, a 2010 study concluded that patients with ACS or atrial fibrillation respond well to clopidogrel, regardless of CYP2C19 loss-of-function carrier status.
Ticlopidine (Ticlid)
Beneficial effects were noted in patients with UA after 2 wk of use in one randomized trial. When compared to controls, ticlopidine use decreased vascular deaths and nonfatal MIs.
Prasugrel (Effient)
Thienopyridine drug that inhibits platelet activation and aggregation through the irreversible binding of its active metabolite to ADP platelet receptors (specifically the P2Y12 receptor). Platelet inhibition is the result of this action.
Indicated to reduce thrombotic cardiovascular (CV) events (including stent thrombosis) with acute coronary syndrome (ACS) that is managed with percutaneous coronary intervention (PCI). Specifically for unstable angina or non – ST-elevation myocardial infarction (NSTEMI) or with ST-elevation myocardial infarction (STEMI) when managed with primary or delayed PCI.
Reduces rate of combined endpoint of CV death, nonfatal MI, or nonfatal stroke compared with clopidogrel.
Ticagrelor (Brilinta)
Ticagrelor and its major metabolite reversibly interact with the platelet P2Y12 ADP-receptor to prevent signal transduction and platelet activation. Indicated to reduce the rate of thrombotic cardiovascular events in patients with ACS (unstable angina, non-ST elevation MI, or ST elevation MI).
Clinical trial results showed a reduced rate of combined endpoint of cardiovascular death, MI, or stroke compared to clopidogrel. Difference between treatments was driven by CV death and MI with no difference in stroke. In patients treated with PCI, ticagrelor also reduces the rate of stent thrombosis.
The drug is administered with aspirin (loading dose of 325 mg PO once, then 75-100 mg/day). Note that exceeding an aspirin dose of 100 mg/day decreases ticagrelor effectiveness.
 RSS Feed
RSS Feed Twitter
Twitter



 Sunday, March 29, 2015
Sunday, March 29, 2015
 Unknown
Unknown
 Posted in
Posted in
Heparin-degrading lyase that recognizes heparin sulfate proteoglycan as its primary substrate. Heparinase I and III plays vital role in various biological processes: heparinase
ReplyDeleteHeparin-degrading lyase that recognizes heparin sulfate proteoglycan as its primary substrate. Heparinase I and III plays vital role in various biological processes: modulate cell-growth factor interactions, heparinase
ReplyDeleteI started on COPD Herbal treatment from Ultimate Health Home, the treatment worked incredibly for my lungs condition. I used the herbal treatment for almost 4 months, it reversed my COPD. My severe shortness of breath, dry cough, chest tightness gradually disappeared. Reach Ultimate Health Home via their email at ultimatehealthhome@gmail.com . I can breath much better and It feels comfortable!
ReplyDelete